SSRI vs. SNRI: Key Differences, Benefits, and Side Effects (January 2026)
SSRI vs SNRI: Differences & Benefits (Jan 2026)
Written by:

Arthur MacWaters
Founder, Legion Health
If you are comparing SSRI vs SNRI options, the choice usually depends on your specific symptoms and how your body responds to treatment. SSRIs increase serotonin to help steady mood and anxiety, while SNRIs also increase norepinephrine, which can support energy and sometimes help with certain pain conditions. Both medication classes are considered first‑line treatments for depression and many anxiety disorders, and it is common to try one and then switch if it is not a good fit.
TLDR:
SSRIs primarily target serotonin for mood support; SNRIs act on both serotonin and norepinephrine, which can influence energy and some types of pain.
Weight gain affects many long‑term users (around 55–65 percent), and both classes can cause sexual side effects.
SNRIs are more likely to raise blood pressure and can be harder to taper off than many SSRIs.
Legion Health offers insurance‑covered psychiatric evaluations to help you find the medication approach that fits you best.
What Are SSRIs and SNRIs

Sorting through medication options can feel confusing. These are the core differences between SSRIs and SNRIs.
SSRIs (Selective Serotonin Reuptake Inhibitors) focus on serotonin.
SNRIs (Serotonin‑Norepinephrine Reuptake Inhibitors) affect both serotonin and norepinephrine.
Both are commonly used first‑line for depression and anxiety.
The main distinction is how they work in the brain. SSRIs (such as Zoloft or Lexapro) act primarily on serotonin, which influences mood and emotional processing. SNRIs (such as Effexor or Cymbalta) act on both serotonin and norepinephrine, a neurotransmitter linked to energy, alertness, and pain pathways. Because of this dual effect, clinicians often consider SNRIs when depression or anxiety shows up alongside fatigue, low motivation, or certain kinds of chronic pain.
Both classes work by reducing the reuptake of these neurotransmitters so they remain active in the brain for longer. SSRIs account for 42% of all antidepressant prescriptions and the median duration of antidepressant use in the United States is approximately 5 years, vastly exceeding the 8 week median trial duration used in clinical studies.
How SSRIs and SNRIs Work Differently
SSRIs target serotonin, a neurotransmitter responsible for managing mood, sleep, and emotional processing. Increasing serotonin levels is often effective for stabilizing general symptoms of anxiety and depression.
SNRIs differ by also inhibiting the reuptake of norepinephrine. This chemical influences energy, focus, and alertness. Due to this dual mechanism of action, SNRIs are often considered when a patient experiences physical pain, fatigue, or low motivation in addition to mood changes.
Both SSRIs and SNRIs are treatments for major depressive disorder and generalized anxiety disorder. Since their overall effectiveness is similar, the decision usually comes down to co‑occurring symptoms and side‑effect profiles.
SSRI Strengths
SSRIs are often the first choice for conditions involving intrusive thoughts, such as OCD, PTSD, and social anxiety disorder. Clinicians frequently prefer them when someone has strong worry, rumination, or trauma‑related symptoms and wants a lower chance of physical “activation” that can sometimes show up with norepinephrine.
SNRI Strengths
SNRIs are often chosen when physical symptoms are common alongside mood issues. Some SNRIs are FDA‑approved for chronic musculoskeletal pain and fibromyalgia, and can be helpful when depression occurs together with pain, low energy, or lethargy.
Comparison of Common Uses
Condition | SSRIs | SNRIs |
|---|---|---|
Depression (MDD) | First-line treatment | First-line treatment |
Generalized Anxiety (GAD) | First-line treatment | First-line treatment |
OCD | Frequently prescribed | Second-line or off-label |
PTSD | First-line treatment | Second-line or off-label |
Panic Disorder | First-line treatment | FDA-approved |
Chronic Pain / Fibromyalgia | Not typically used | FDA-approved |
Clinicians look at the full symptom profile to decide. Depression with OCD tends to point toward an SSRI, while depression with chronic pain may point toward an SNRI.
SSRI vs SNRI for Depression
Effectiveness and Response Rates
Studies suggest that both SSRIs and SNRIs provide similar overall benefit for many people with depression and anxiety, with some data showing slightly higher effect sizes for SNRIs in severe depression. In practice, the best choice is usually the medication you can tolerate and stay on, not the one that looks marginally better in a pooled analysis.
Clinical Selection
SSRIs are often used first because they have been widely studied, are familiar to clinicians, and generally have a manageable safety profile. An SNRI may be recommended if you have chronic fatigue, physical pain, or if you have tried an SSRI without adequate benefit. Switching from an SSRI to an SNRI is a common next step when response is partial or minimal.
SSRI vs SNRI for Anxiety
For generalized anxiety, panic disorder, and social anxiety, both SSRIs and SNRIs are considered appropriate first‑line options with comparable effectiveness. The decision often depends on your specific symptom mix, your medical history, and how sensitive you are to side effects.
Because SNRIs also increase norepinephrine, they can lead to physical sensations such as jitteriness, sweating, or a faster heart rate, especially when starting or increasing the dose. These feelings can resemble panic symptoms, which is one reason clinicians often begin with an SSRI when anxiety is the main problem. An SNRI may be considered if you do not respond well to an SSRI or if your anxiety occurs alongside low energy or certain pain conditions.
Common Side Effects: SSRI vs SNRI
Since both medication classes influence serotonin, they share many side effects, including nausea, headaches, changes in sleep, and sexual side effects. These often improve within several weeks as your body adjusts, but not always.
Weight Gain
Weight changes are a common concern when thinking about SSRI vs SNRI weight gain. A recent review estimated that roughly 55–65 percent of people on long‑term antidepressant therapy experience some degree of weight gain over time. Within SSRIs, paroxetine (Paxil) is frequently linked with higher rates of weight gain, while fluoxetine (Prozac) is often associated with lower risk.
Unique SNRI Risks
SNRIs affect norepinephrine, which can lead to physical side effects less common with SSRIs, such as higher blood pressure, increased sweating, dry mouth, and constipation. For this reason, clinicians often check blood pressure before and during SNRI treatment, especially in people with a history of hypertension.
If side effects remain troublesome beyond the usual adjustment period, your clinician may adjust the dose or recommend a different medication.
Sexual Side Effects
Because both SSRIs and SNRIs increase serotonin, they can reduce dopamine activity tied to desire and arousal. Many people notice lower libido or difficulty reaching orgasm on either class, and the overall risk is relatively similar across them.
Emotional Blunting
Some people describe feeling “numb” or emotionally flat on these medications. Reports suggest this is often more about how high the dose is and the individual’s sensitivity than about a single class being uniquely responsible. It can also overlap with residual depression or burnout, so it is important to talk through what you are experiencing with your clinician.
Discontinuation Symptoms
Stopping antidepressants too quickly can lead to discontinuation symptoms in an estimated 20 percent of people, including dizziness, nausea, sensory changes, and sleep disruption. The risk is higher with shorter half‑life medications such as paroxetine (SSRI) and venlafaxine (SNRI). SNRIs are often described as more challenging to taper because of withdrawal‑like symptoms when doses are reduced too abruptly. To reduce discomfort, clinicians usually recommend a gradual tapering schedule instead of stopping all at once.
If sexual side effects, emotional blunting, or discontinuation symptoms are affecting your daily life, your clinician may lower the dose, switch to a different SSRI or SNRI, or in some cases consider adding a dopamine‑targeting agent such as an NDRI.
NDRIs: Another Antidepressant Option
DRIs (Norepinephrine‑Dopamine Reuptake Inhibitors), such as bupropion (Wellbutrin), act on norepinephrine and dopamine, which influence alertness, motivation, and reward. Unlike serotonin‑based options, NDRIs are less likely to cause sexual dysfunction or weight gain for many people.
Clinicians may combine an SNRI and an NDRI to support energy and offset certain sexual side effects, depending on your history and risk factors. For people with chronic anxiety, SSRIs are often preferred because NDRIs can sometimes increase agitation or restlessness. NDRIs are also not appropriate for people with seizure disorders or certain eating disorders.
Choosing Between SSRIs, SNRIs, and NDRIs
Deciding “SSRI vs SNRI, which is better” depends on your specific symptom pattern. SSRIs are frequently chosen when anxiety, intrusive thoughts, or rumination are at the forefront. SNRIs may be a better match when there is marked fatigue, low energy, or co‑occurring pain, since norepinephrine can influence both mood and physical energy. NDRIs sometimes enter the picture when low motivation is common and avoiding sexual side effects or weight gain is a priority.
The SSRI vs SNRI vs NDRI choice also depends on how you tolerate medications and what has worked for you or family members in the past. If a close relative had a good response to a particular medication, that information can help guide selection. Your clinician will also factor in medical conditions such as high blood pressure, seizure history, and sleep patterns.
Getting Started With Psychiatric Medication Management
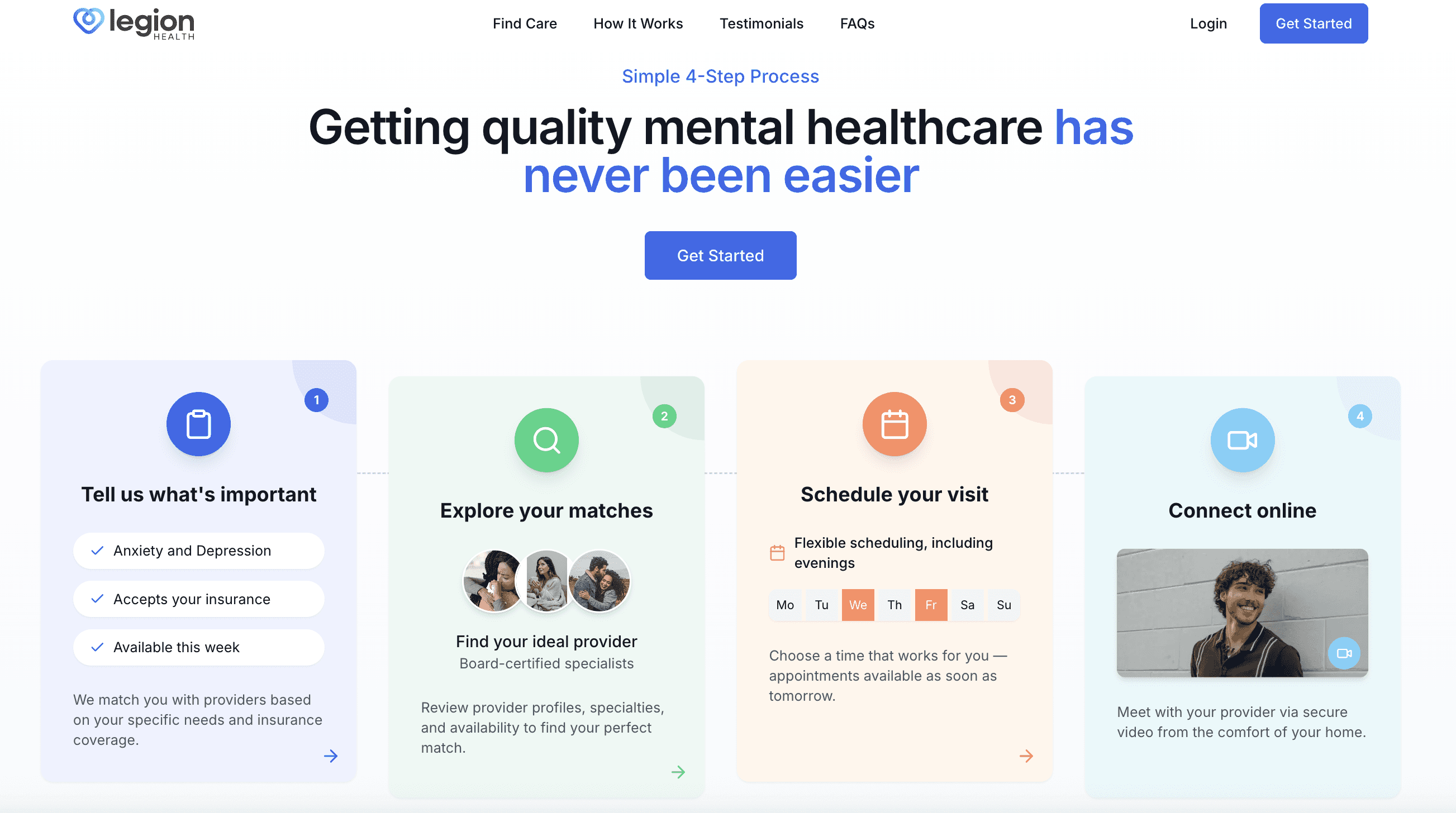
Sorting out whether you need more serotonin support, norepinephrine support, or a combination is not something you have to figure out alone. Because symptoms often overlap and evolve, choosing the right medication usually requires a detailed evaluation by a p
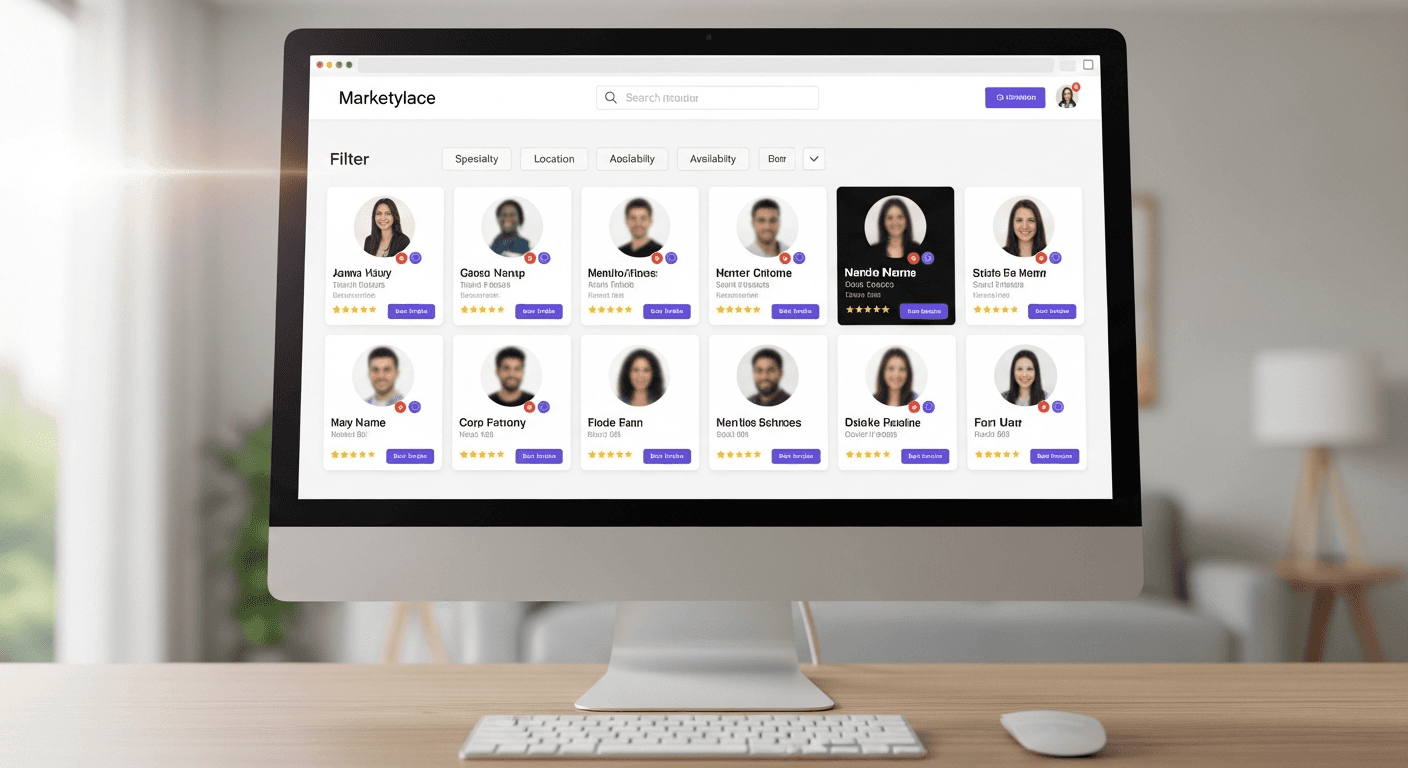
At Legion Health, psychiatric care is delivered virtually and is designed to be insurance‑friendly and accessible. Our clinical team reviews your full history, including past medication trials, other health conditions, and current goals to decide whether an SSRI, SNRI, NDRI, or another option is the safest path. Care does not stop after the first visit. Follow‑ups are built in so side effects can be monitored and doses adjusted until you reach a more stable place.
Get matched with a licensed clinician who accepts your insurance.
Receive a careful evaluation and a clear treatment plan.
Start ongoing care with predictable follow‑ups.
If you want a clear plan for your symptoms, the next step is a psychiatric evaluation. You can see if Legion Health is a fit and schedule your first visit.
Final Thoughts on SSRI vs SNRI Treatment Options
Choosing between SSRI vs SNRI comes down to matching your symptoms and health history with the mechanism that fits best. SSRIs focus on serotonin and are often a strong choice for anxiety, intrusive thoughts, and many depressive symptoms, while SNRIs add norepinephrine support that can help when energy, concentration, or certain pain conditions are part of the picture. Both require time, monitoring, and adjustment. If you are ready to see which option fits your situation, a psychiatric evaluation is the next step
FAQs
What is the main difference between SSRIs and SNRIs?
SSRIs increase serotonin to support mood and emotion, while SNRIs increase both serotonin and norepinephrine, which can also affect energy and some pain pathways. This makes SNRIs a common choice when fatigue or chronic pain show up with depression or anxiety.
Which medication class is better for anxiety: SSRI or SNRI?
Both are considered first‑line treatments for many anxiety disorders, and overall effectiveness is similar. SSRIs are often used first because SNRIs can sometimes cause physical activation, such as jitteriness or sweating, that may feel similar to panic.
Can SNRIs help with chronic pain as well as depression?
Yes. Certain SNRIs are FDA‑approved for chronic musculoskeletal pain and fibromyalgia, reflecting norepinephrine’s role in pain signaling. They are commonly used when depression occurs alongside these conditions.
Do SSRIs or SNRIs cause more weight gain?
Both classes have similar long‑term weight gain risk overall, though individual medications differ. Paroxetine is often associated with higher risk, while fluoxetine tends to show lower weight gain in studies.
Are SNRIs harder to stop than SSRIs?
SNRIs are often described as more challenging to discontinue, especially shorter‑acting ones like venlafaxine, because they can cause more noticeable discontinuation symptoms if stopped quickly. Your clinician will usually recommend a gradual taper to reduce these effects.
We're honored to support thousands on their journeys. Here's what some have shared: