Best Mental Health Platforms with Outcome Tracking (December 2025)
Outcome-Tracking Mental Health Platforms Dec 2025
Written by:

Arthur MacWaters
Founder, Legion Health
Picking a mental health provider usually comes down to convenience and cost. But if your provider isn't tracking your symptoms with standardized tools, you might spend months on a medication that barely helps while better options exist. Treatment effectiveness measurement turns psychiatric care from educated guessing into evidence-based adjustments, catching stalled progress weeks earlier than subjective check-ins alone. This comparison looks at how different telepsychiatry services approach outcome tracking and what that means for your results.
TLDR:
Outcome tracking improves psychiatric treatment response rates by 20-30% vs standard care
Legion Health uses standardized assessments at every visit plus free QbCheck ADHD testing
Insurance-based care requires documented progress, creating accountability cash-pay lacks
Ask providers which specific tools they use and how often you'll complete assessments
Legion Health serves Texas with board-certified providers, insurance coverage, and data-driven care
SEO Optimized Outline for: Top Outcome-Tracking Mental Health Platforms (November 2025 Update)
Outcome tracking in mental health has shifted from academic research to clinical standard. Most psychiatric services still rely on subjective symptom reports rather than standardized measurement tools.
This guide compares telepsychiatry providers based on their measurement-based care practices. We'll examine how Legion Health, Talkiatry, and others approach outcome monitoring, what tools they use, and how their models affect treatment accountability.
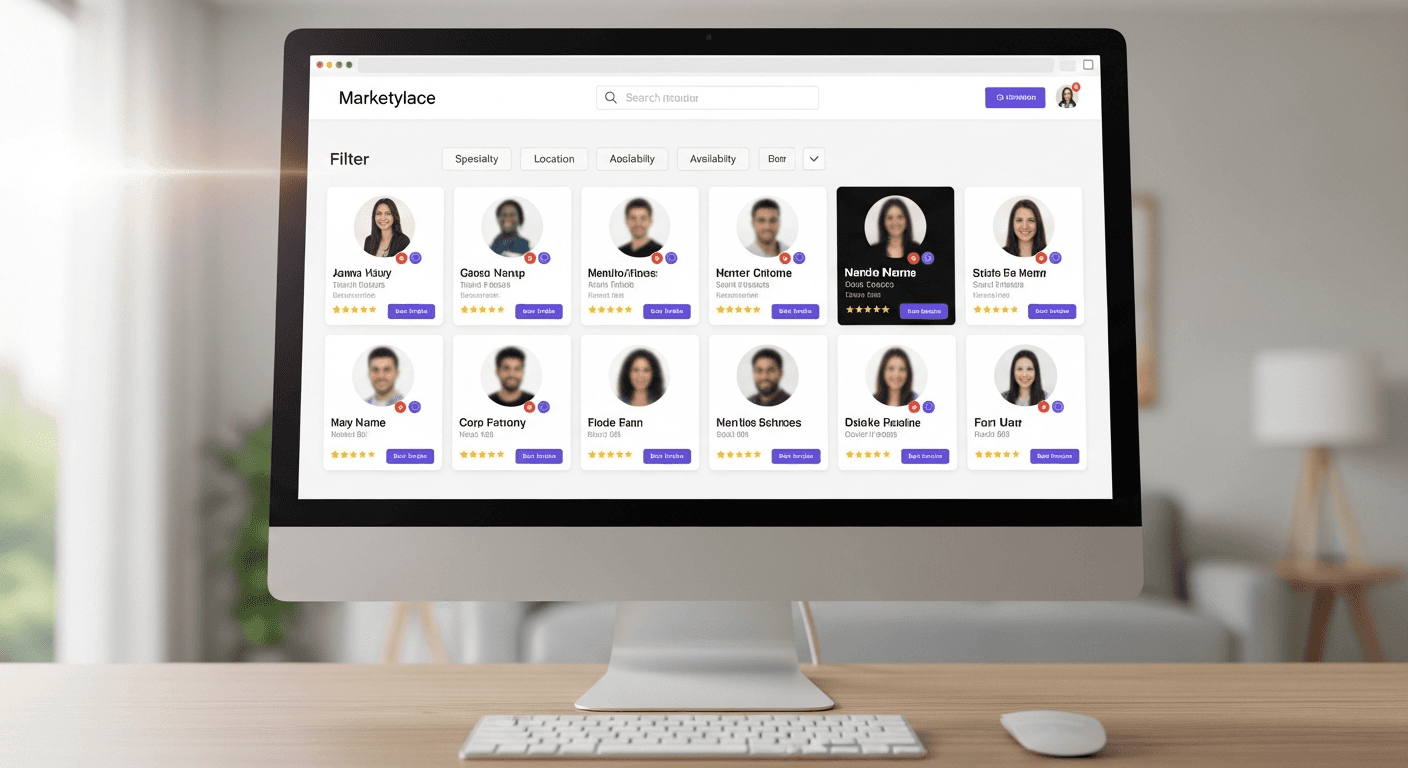
Provider | Outcome Tracking Approach | Assessment Frequency | Objective Testing | Insurance Model | Key Limitations |
|---|---|---|---|---|---|
Legion Health | Standardized assessments (PHQ-9, GAD-7) at every visit with scores reviewed against baseline data | At intake and all follow-up visits | Free QbCheck ADHD testing with unlimited retesting during treatment | Accepts all major commercial insurance plans in Texas, creating accountability through documented progress | Texas-only availability |
Talkiatry | Standard intake assessments and symptom questionnaires with protocols varying by provider | Varies by individual provider | No objective ADHD testing like QbCheck included | Insurance-based with board-certified providers | Limited in-network options in Texas, appointments book several weeks out, inconsistent measurement protocols |
Cerebral | Subscription-based model with less external pressure for standardized tracking | Not systematically documented | Not specified | Monthly subscription $99-$325 out-of-pocket regardless of insurance | Cash-pay structure lacks insurance accountability for documented outcomes |
Brightside Health | Outcome monitoring for depression and anxiety only | Not systematically documented | No objective testing tools | Hybrid model with select insurance plans and cash-pay options | Does not treat ADHD, limited state availability, no objective measurement tools |
Mindpath Health | Inconsistent protocols across multiple locations and providers | Varies by location and clinician preference | Not systematically documented | Hybrid in-person and virtual with insurance coverage | Lack of uniform measurement protocols across dispersed offices, traditional practice structure makes consistent tracking difficult |
Systematic outcome tracking improves response rates by 20-30% compared to standard care. Understanding a provider's measurement approach helps you get better results for anxiety, depression, or ADHD treatment.
What is Outcome Tracking in Mental Health Care
Outcome tracking uses validated assessment tools to measure symptom severity and treatment progress. Instead of relying on memory or subjective impressions, clinicians give standardized questionnaires at regular intervals during care.
These tools generate quantifiable data about specific symptoms. Depression scales score mood, sleep, and energy levels numerically. Anxiety inventories measure worry intensity and physical symptoms. ADHD assessments evaluate attention span, impulsivity, and hyperactivity through structured questions.
The scores create a timeline of treatment response. If your depression score drops from 18 to 7 over two months, you and your provider see concrete evidence your medication works. If scores plateau or worsen, that signals a need to adjust treatment before more time passes.
Why Measurement-Based Care Adoption Remains Below 20%
Fewer than 20% of mental health providers use systematic outcome tracking. Time pressure explains part of the gap. Clinicians already manage full schedules, and adding questionnaires feels like one more task competing for limited appointment time.
Workflow friction creates barriers. Paper forms need manual scoring and storage. Digital tools require training and rarely sync with existing electronic health records. Solo practitioners face these challenges without administrative staff to manage implementation.
Training gaps matter too. Many clinicians learned psychiatry without measurement-based protocols and rely on clinical judgment alone. They see standardized scales as optional rather than central to treatment quality.
Core Benefits of Data-Driven Psychiatry for Patient Outcomes
Data-driven psychiatry catches treatment failures weeks earlier than relying on subjective check-ins. When scores show stalled progress at week four, providers adjust medication immediately rather than waiting months while symptoms persist.
Patients receiving measurement-based care achieve up to 75% greater remission rates compared with treatment without routine symptom measurement. Objective data removes guesswork from deciding whether your current regimen works or needs adjustment.
Tracking also validates experience. If you feel only slightly better but your depression score dropped 40%, you gain confidence that treatment progresses even when recovery feels slow.
Standard Assessment Tools Used for Psychiatric Outcome Monitoring
The PHQ-9 and GAD-7 became the dominant psychiatric screening tools because they're brief, free, and validated across populations. The PHQ-9 tracks depression symptoms over two weeks through nine questions, producing scores from 0 to 27. GAD-7 follows the same structure for anxiety with seven questions about worry and physical tension.
Both assessments take under three minutes, allowing clinicians to readminister them at each visit without adding burden. At intake, a PHQ-9 score of 16 signals moderately severe depression and creates a numeric baseline. After six weeks of medication, a drop to 8 confirms treatment response and informs dosing decisions.
What is Legion Health
Legion Health is a Texas telepsychiatry service founded in 2021 that delivers medication management for anxiety, depression, and ADHD through virtual appointments.
We accept all major commercial insurance plans across Texas, covering roughly 95% of commercially insured Texans.

Care comes from board-certified psychiatric providers who can typically see new patients within days. Appointments happen via video, with evening slots available to fit work schedules.
We handle the full scope of psychiatric medication management, from initial evaluation through ongoing follow-ups and treatment adjustments. Prescriptions go electronically to your pharmacy immediately after appointments. Most patients pay only their insurance copay per visit.
How Legion Health Integrates Outcome Measurement Into Care
We give standardized symptom assessments at intake and throughout treatment to track progress numerically. These include depression and anxiety scales alongside condition-specific measures that match your diagnosis.
Every follow-up visit reviews your latest scores against baseline data. If your anxiety severity dropped from 14 to 6 over two months, that shows evidence your medication regimen works. Scores that plateau or rise trigger immediate treatment adjustments rather than waiting for you to report worsening symptoms.
For ADHD care, we use QbCheck evaluations that measure attention, impulsivity, and activity objectively through computerized testing. You can retake QbCheck at no cost during follow-ups to quantify how treatment affects specific ADHD symptoms over time.
QbCheck Testing for Objective ADHD Outcome Data
QbCheck is an FDA-cleared computerized test that measures attention, impulsivity, and activity during a 15-20 minute task. The test compares results against normative data for age and sex, providing objective performance metrics rather than relying solely on self-reported questionnaires.
QbCheck enables retesting during treatment to track changes in measurable outcomes. A patient whose inattention score moves from the 5th percentile to the 40th percentile after medication adjustment has quantifiable evidence that the regimen is working beyond what symptom checklists can capture.
Talkiatry's Approach to Treatment Effectiveness Measurement
Talkiatry runs an insurance-based telepsychiatry service with board-certified psychiatric providers.
The service includes standard intake assessments and symptom questionnaires, though measurement protocols differ depending on which provider you see.
Appointments usually book out several weeks. The service does not include objective ADHD testing like QbCheck for evaluations or ongoing monitoring.
Texas patients may find more limited in-network insurance options. Coverage restrictions can affect both access and the clinical accountability that insurance-based reimbursement requires through documented outcomes.
Cerebral's Subscription Model vs. Outcomes-Focused Insurance Care
Cerebral operates on a monthly subscription model starting around $99-$325 per month depending on services. Members pay out-of-pocket regardless of insurance coverage, creating a direct consumer relationship rather than reimbursement accountability to insurers.
Subscription models prioritize member retention over documented clinical improvement. Insurance-based care requires providers to justify medical necessity through assessment data and progress notes that payers audit regularly. Cash-pay services face less external pressure to show measurable outcomes through standardized tracking tools.
This structural difference affects measurement frequency. Insurance billing incentivizes regular symptom monitoring because payers expect documentation showing treatment remains medically appropriate.
Insurance Coverage and Accountability Differences
Insurance companies demand proof that treatment remains medically necessary at each appointment. Payers review claims and reject payment when records fail to document symptom severity, treatment response, and the rationale for ongoing care. These audit requirements create built-in pressure for outcome tracking.
When submitting claims, we include outcome data with billing codes to show clinical improvement. For example, if depression scores remain unchanged after eight weeks, we either modify treatment or document why continuing the current approach makes sense. Patients who pay out-of-pocket each month don't trigger this same accountability mechanism.
Brightside Health's Outcome Monitoring Capabilities
Brightside Health offers telepsychiatry for depression and anxiety through a hybrid payment model that includes select insurance plans and cash-pay options. The service operates in limited states with a scope restricted to mood and anxiety disorders.
Brightside does not treat ADHD or include objective testing tools for outcome measurement. Patients seeking quantifiable progress monitoring or care for conditions beyond mood and anxiety disorders will need to consider other providers.
Mindpath Health's Hybrid In-Person and Virtual Care Model
Mindpath Health runs a multi-state group practice offering both in-person and virtual appointments. This hybrid structure creates challenges for standardized outcome tracking across locations.
Traditional practices with multiple offices often lack uniform measurement protocols. Different locations may use different assessment tools or skip systematic tracking when clinician preferences vary across the organization.
Telehealth-first services integrate outcome measurement into their workflows from the start. Hybrid practices add tracking systems to existing operations, making consistent data collection harder across dispersed teams.
Key Features to Evaluate in Outcome-Tracking Mental Health Services
Assessment frequency matters most. Services committed to measurement-based care give you standardized tools at intake and every follow-up, not occasionally when someone thinks of it. Ask directly how often you'll complete symptom questionnaires.
Your outcome data should shape clinical decisions. Providers who genuinely use measurements will reference your scores during visits and explain how results inform medication adjustments. When clinicians never mention your assessment results, the tracking exists only for documentation.
Check if objective testing supplements self-report measures. For ADHD, computerized performance tests like QbCheck add quantifiable data beyond symptom checklists. Few services include objective testing without extra fees.
Make sure you'll see your own results. Transparent services share scores and trends so you understand your progress numerically and can participate actively in treatment planning.
How Outcome Data Improves ADHD Medication Safety and Effectiveness
Outcome data turns ADHD medication management into precise dosing decisions. Baseline QbCheck scores measure attention and impulsivity before treatment begins, creating an objective standard for tracking medication response. Follow-up testing shows whether your current dose improves performance or requires adjustment.
Side effect monitoring catches problems early. Regular symptom tracking identifies sleep disruption, appetite changes, or anxiety spikes before they worsen. When scores decline despite medication, providers distinguish between inadequate dosing and tolerance.
This measurement approach supports responsible stimulant prescribing. Documented improvement justifies continuing controlled substances, while lack of progress triggers reevaluation. Objective evidence maintains both clinical safety and treatment accountability.
What to Ask Providers About Their Outcome Measurement Process
Ask which specific assessment tools they use by name. Generic answers like "we track symptoms" don't confirm validated instruments. Look for PHQ-9, GAD-7, or other standardized scales rather than informal check-ins.
Find out how often you'll complete assessments. Quality measurement-based care means repeating tools at every visit or monthly, not just at intake. Irregular tracking won't catch treatment problems early.
For ADHD specifically, ask whether they offer objective testing beyond questionnaires. Most providers rely entirely on self-report scales. Services with QbCheck or similar computerized tests provide quantifiable attention and impulsivity data.
Confirm that outcome data directly affects your treatment plan. Ask how results from assessments change medication decisions. Providers should explain how your scores determine dose adjustments, medication switches, or treatment timelines.
Question what happens if your scores show minimal improvement after two months. Strong programs have protocols for treatment changes when data indicates poor response rather than continuing ineffective regimens indefinitely.
Final thoughts on evidence-based telehealth for mental health
Evidence-based telehealth with systematic outcome measurement gives you accountability that cash-pay services often skip. Insurance-based care requires documented progress at every visit, creating built-in pressure for providers to track your symptoms and adjust treatment when scores plateau. If you're managing depression, anxiety, or ADHD, measurement-based care turns your treatment into a data-informed process rather than trial and error.
FAQ
How often should I expect to complete symptom assessments during treatment?
Quality measurement-based care includes standardized assessments at intake and every follow-up visit, typically monthly or more frequently during medication adjustments. If a provider only gives you questionnaires at your first appointment, they're not using outcome data to guide your ongoing treatment decisions.
What's the difference between self-report questionnaires and objective ADHD testing?
Self-report questionnaires like rating scales capture your perception of symptoms, while objective tests like QbCheck measure actual attention performance, impulsivity, and activity through computerized tasks. Objective testing provides quantifiable data independent of memory or subjective impressions, giving your provider concrete evidence of how treatment affects measurable ADHD symptoms.
Can outcome tracking help catch medication side effects earlier?
Yes—regular symptom monitoring identifies problems like sleep disruption, appetite changes, or increased anxiety within weeks rather than months. When your assessment scores decline despite medication, your provider can distinguish between inadequate dosing, emerging side effects, or medication tolerance, then adjust treatment before issues worsen.
Why do insurance-based providers track outcomes more consistently than cash-pay services?
Insurance companies require documented proof that treatment remains medically necessary at each visit through symptom severity data and progress notes. Payers audit claims and reject payment when records lack outcome documentation, creating built-in accountability for measurement-based care that monthly subscription models don't face.
What should I do if my provider never discusses my assessment scores during appointments?
Ask directly how your latest scores compare to baseline and what they mean for your treatment plan. Providers committed to measurement-based care will reference your data when explaining medication decisions. If they can't answer or dismiss the question, the assessments exist only for documentation rather than guiding your care.
We're honored to support thousands on their journeys. Here's what some have shared: